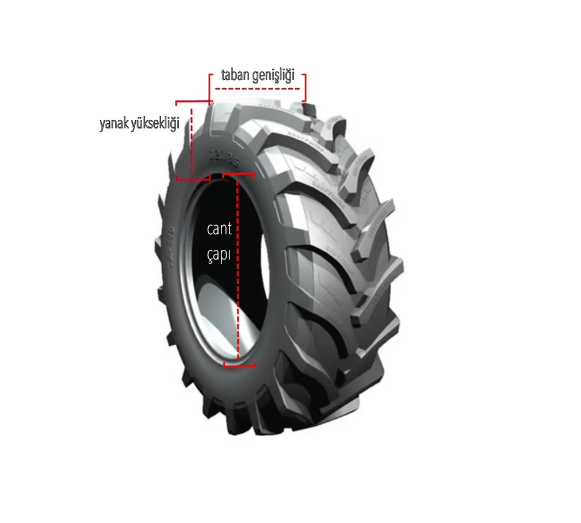
AHLAS LASTİK KAPLAMA - 640 FİAT TRAKTÖR ÖN LASTİGİ 750 * 16 PETLAS OLUKLU DESEN KAPLAMASİ ARKA LASTİGİ 16.9-14*30 LASSA TRAKTÖR DESEN KAPLAMASİ | Facebook
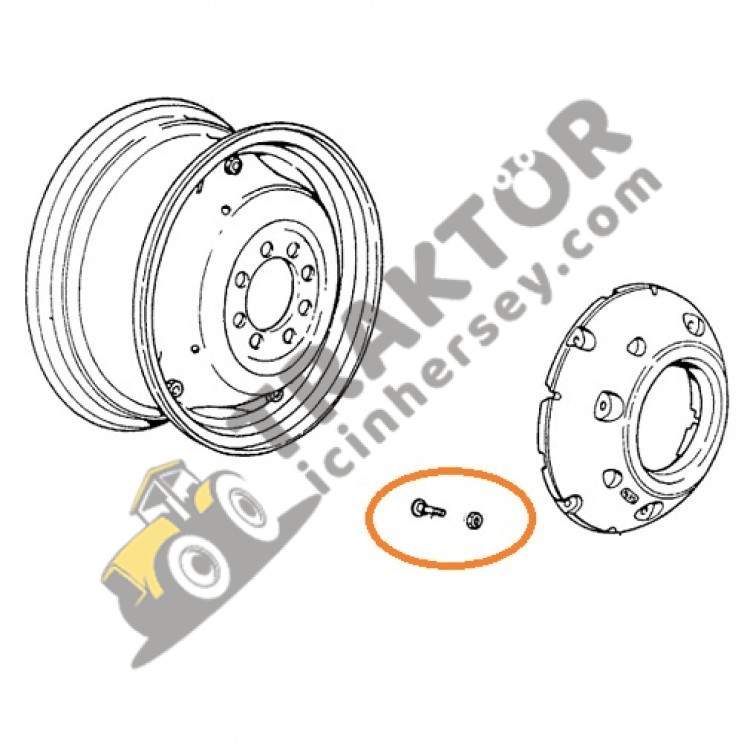
Arka Teker Ağırlık Civatası Kare Başlı Somunlu Fiat 415-450-480-540-640 Ekonomi OC300920181448 - traktorincinhersey.com